Main Functions and Contraindications of Hydrocolloid Dressings
Ⅰ. Hydrocolloid Dressing Definition
Hydrocolloid dressings are dressings made by mixing elastic polymeric hydrogels with synthetic rubber and adhesives. The most common gel used in dressings is hydroxymethylcellulose, which adheres firmly to the skin at the wound edge and swells up to 12 times when it absorbs exudate.
Hydrocolloid dressing is one of new types of medical dressings developed under the guidance of the principle of wet healing. Hydrocolloid dressings can be applied to the treatment of various wounds, especially for chronic refractory wounds. The absorbency and viscosity of hydrocolloid make it meet the basic requirements of an ideal dressing, that is, to protect the wound, provide a suitable environment to promote wound healing, and be easy to remove without damaging the new tissue. Of course, hydrocolloid dressings still have room for further development, such as improving absorbability and enhancing antibacterial ability.
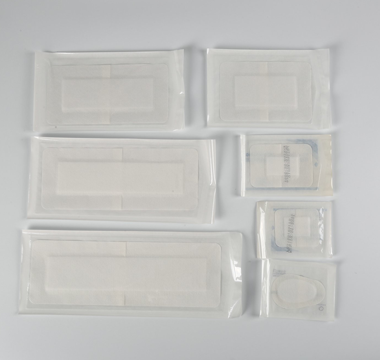
Ⅱ. Types of Hydrocolloid Dressings
There are several types of hydrocolloid dressings available, each designed for specific wound types and healing stages. Here, we explore the most common types of hydrocolloid dressings.
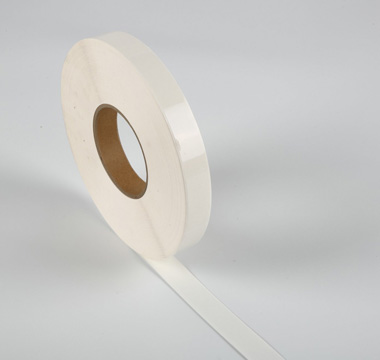
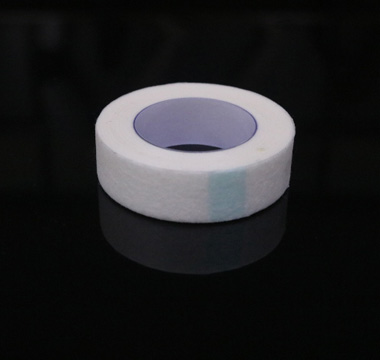
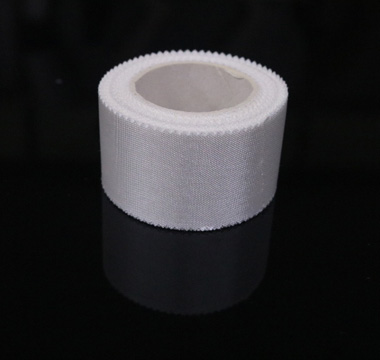
1. Thin Hydrocolloid Dressings
Thin hydrocolloid dressings are designed for managing light to moderately exuding wounds. They are particularly useful for superficial wounds, minor burns, and abrasions. These dressings are flexible and conformable, making them an excellent choice for areas of the body that experience movement. Thin hydrocolloid dressings are also semi-transparent, which allows for wound inspection without the need to remove the dressing.
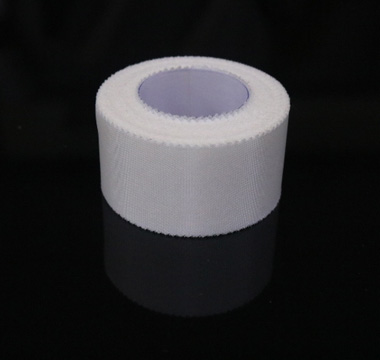
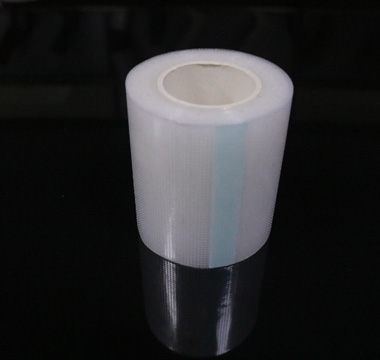
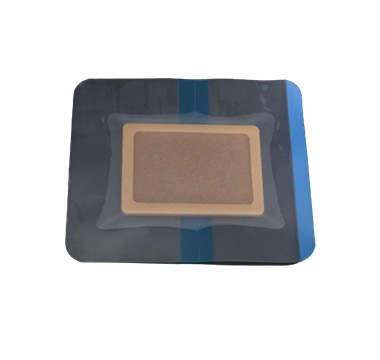
2. Thick Hydrocolloid Dressings
Thick hydrocolloid dressings are intended for moderate to heavily exuding wounds. They are often used on deeper wounds, such as pressure ulcers and leg ulcers, where a higher level of exudate absorption is required. These dressings are more substantial and provide a higher degree of cushioning and protection compared to their thinner counterparts. Due to their thickness, they may not be as conformable, but they are excellent at managing exudate and promoting healing in more severe wounds.
3. Hydrocolloid Dressing with Silver
Some hydrocolloid dressings are impregnated with silver to provide an antimicrobial effect. These dressings are suitable for infected wounds or wounds at high risk of infection. The silver ions released by the dressing can kill a broad spectrum of bacteria, reducing the bacterial load in the wound and promoting a healthier healing environment. These dressings combine the moisture-balancing benefits of traditional hydrocolloids with the added advantage of infection control.
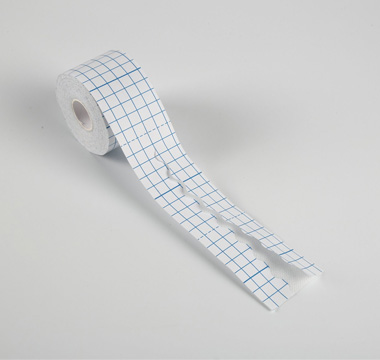
4. Specialty Hydrocolloid Dressings
Specialty hydrocolloid dressings are designed for specific applications or wound types. For example, some are shaped or sized for particular body parts, such as the sacral area. Others are formulated with additional ingredients, such as alginate, to enhance absorption capabilities or to provide other therapeutic benefits. These dressings are tailored to meet the unique needs of certain wounds or to provide additional convenience in wound management.
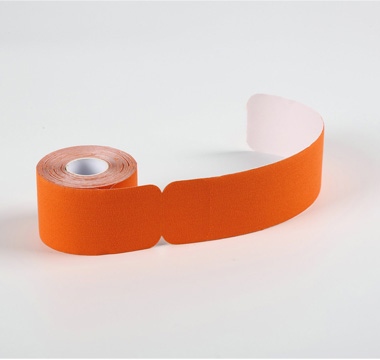
5. Hydrocolloid Dressing Strips
Hydrocolloid dressing strips are narrow strips of hydrocolloid material that are ideal for wrapping around fingers, toes, or other small or awkwardly shaped areas. They are particularly useful for managing blisters, cuts, or abrasions in areas that are difficult to dress with larger, more traditional dressings. These strips provide the same moist healing environment and exudate management as larger hydrocolloid dressings but in a more versatile form.

Ⅲ. Benefits Of Hydrocolloid Wound Dressing
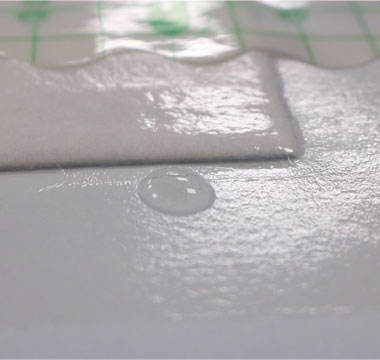
1. Promotes Moist Wound Healing
Hydrocolloid dressings create an optimally moist environment that promotes the natural healing process. Unlike traditional dressings that may dry out the wound, hydrocolloids maintain moisture, which facilitates cell migration, accelerates wound healing, and reduces the risk of scab formation.
2. Protects Against Infection
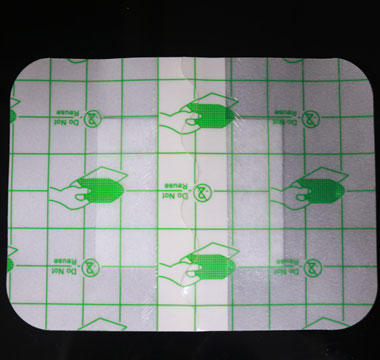
These dressings form a protective barrier over the wound, shielding it from external contaminants, bacteria, and other infection-causing agents. This barrier not only reduces the risk of infection but also helps in maintaining a sterile environment conducive to healing.
3. Self-Adhesive and Easy to Apply
Hydrocolloid dressings are self-adhesive, making them easy to apply and remove. This feature minimizes discomfort and potential damage to the healing tissue, which is especially important for patients with sensitive skin or those who require frequent dressing changes.
4. Extended Wear Time
Due to their moisture-retentive properties and robust infection barrier, hydrocolloid dressings can remain in place for several days, depending on the wound’s condition and exudate levels. This extended wear time reduces the need for frequent dressing changes, making the healing process more convenient and cost-effective.
5. Promotes Autolytic Debridement
Hydrocolloid dressings facilitate autolytic debridement by maintaining a moist environment that helps to break down dead tissue and promote the wound’s natural cleaning process. This gentle method of debridement is less painful and traumatic than mechanical or surgical methods.
6. Versatility
These dressings are suitable for a wide range of wound types, including pressure ulcers, venous leg ulcers, minor burns, and abrasions. Their versatility makes them a valuable tool in various clinical settings, from hospitals to home care.
7. Pain Management
Hydrocolloid dressings can help in reducing pain associated with wounds. The moist environment and protective barrier minimize exposure to air and external irritants, which can significantly alleviate pain during the healing process.
8. Reduces Scarring
By maintaining an optimal level of moisture and promoting efficient healing, hydrocolloid dressings can help to minimize the formation of scars. This is particularly beneficial for patients concerned about the cosmetic appearance of their skin post-healing.
Ⅳ. The main role of hydrocolloid dressings
Hydrocolloid dressings are mainly used on patients' wounds to protect the wounds and promote wound healing. Mainly used for patients with pressure ulcers, the hydrocolloid dressing can be directly attached to the sterilized pressure ulcer wound or the wound that is about to form a pressure ulcer. The colloid dressing has good elasticity and good air permeability, can help the recovery of the wound surface of the pressure ulcer patient, and avoid the continued aggravation of the pressure ulcer wound surface. The specific usage of the hydrocolloid dressing is to debride and disinfect the local wound surface of the patient first, and then directly attach the hydrocolloid dressing to the wound surface after drying. It is not necessary to replace it every day. It is recommended to replace it once every 3 to 5 days. When replacing, pay attention to the recovery. If the wound surface gradually recovers, you can continue to use it; if the wound surface gradually increases, it is recommended to use other methods for treatment to avoid delaying the disease.
Ⅴ. Contraindications of hydrocolloid dressings
Hydrocolloid dressings are not recommended for wounds with severe infection, exposed skeletal tendons and excessive exudate;
Hydrocolloid dressings form gel after contact with wound exudate. When the hydrocolloid dressing is opened, similar purulent substances can be seen in the wound, accompanied by Special odor, sometimes visible color change and swelling phenomenon, which are the substances and odors formed by the decomposition of the dressing itself and the protein in the exudate;
It cannot be used for superficial to full-thickness wounds, wounds with moderate to large amount of exudate;
For wounds with excessive growth of granulation tissue and a large amount of exudate, foam dressings can be used to make use of its strong exudate. The liquid absorption capacity keeps the local moist and clean, and the elastic bandage is used to inhibit the proliferation of granulation tissue;
Keep the wound moist and the surrounding skin dry to avoid affecting the repair of the wound due to excessive and frequent replacement of hydrocolloid dressings.
Ⅵ. How to Use Custom Hydrocollid Dressing
Step 1: Assess and Prepare the Wound
Before applying a hydrocolloid dressing, carefully assess the wound and the surrounding skin. The wound should be cleaned with a gentle saline solution or wound cleanser to remove any debris or exudate. Ensure the skin around the wound is dry to help the dressing adhere properly. If the wound is deep, has tunneling, or is heavily exuding, a hydrocolloid dressing may not be the best choice, and other wound care options should be considered.
Step 2: Choose the Right Size
Select a custom hydrocolloid dressing that adequately covers the wound and extends at least 1 inch beyond the edges of the wound. This ensures that the dressing can adhere well to the surrounding skin, creating a secure seal. If the dressing does not perfectly match the wound’s shape, it can be cut to size, leaving enough margin to cover the surrounding healthy skin.
Step 3: Apply the Dressing
Peel away the protective backing to expose the adhesive side of the dressing. Carefully position the dressing over the wound, making sure not to stretch it, as this can cause tension on the skin. Start applying the dressing from one side and gently smooth it over the wound, pressing down on the edges to ensure a good seal. Avoid any wrinkles or air bubbles, as these can reduce the effectiveness of the dressing.
Step 4: Monitor and Change the Dressing
Hydrocolloid dressings are designed to be left in place for several days, up to a week, depending on the wound’s condition and the amount of exudate. Monitor the dressing regularly for signs of leakage or loosening. If the dressing becomes saturated, it should be changed. When removing the dressing, do so gently to avoid damaging the new tissue. Clean the wound as per step 1 before applying a new dressing.
Step 5: Document and Evaluate
Keep a record of each dressing change, noting the condition of the wound and any changes observed. This documentation is crucial for evaluating the effectiveness of the treatment and making any necessary adjustments.
Tips for Effective Use
Ensure the skin around the wound is free from creams or oils before applying the dressing, as these can interfere with adhesion.
For wounds with irregular shapes, hydrocolloid dressings can be overlapped to ensure complete coverage.
If the wound is in a difficult-to-dress area, such as a joint, consider using a secondary dressing or medical tape to secure the hydrocolloid dressing in place.
Using custom hydrocolloid dressings effectively can significantly contribute to wound healing by maintaining a moist environment, protecting the wound from infection, and minimizing pain. By following these steps and tips, caregivers and patients can optimize the healing process for a variety of wounds.
Related Fuluo Tape Products
Realted Artice


 中文
中文