Instructions for use of Dispensing Wound Dressing
Dispensing wound dressing typically involves applying a sterile dressing to a wound to promote healing and protect it from infection.
Here are general instructions on how to properly dispense and apply a wound dressing:
- Materials Needed
- Sterile gloves
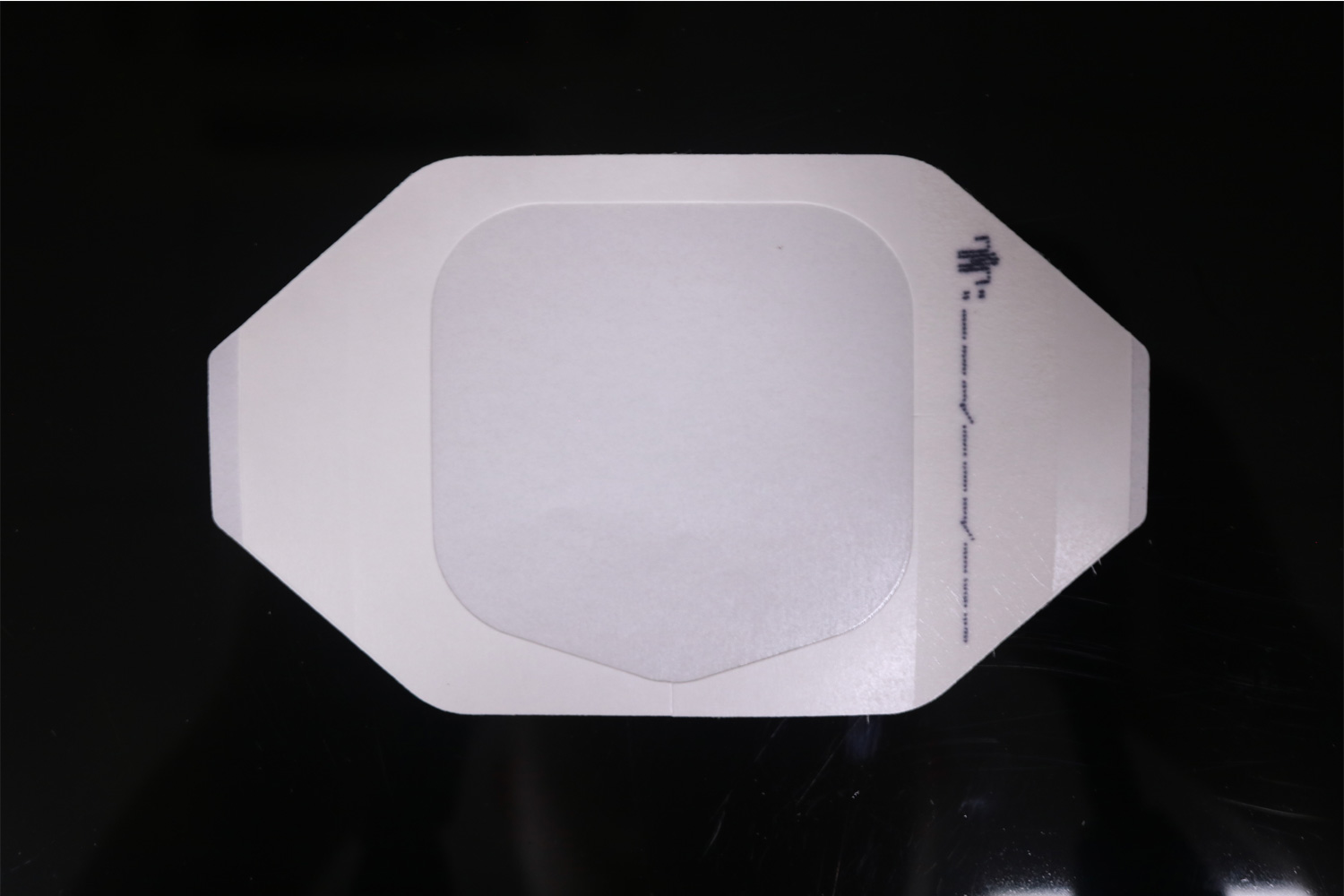
- Sterile dressing (gauze pads, non-stick pads, or specialized dressings like hydrocolloid or foam dressings)
- Sterile saline or wound cleanser
- Adhesive tape or bandage (if needed to secure the dressing)
- Scissors (optional, if cutting the dressing)
- Waste disposal container (for used materials)
Steps for Dispensing Wound Dressing
1. Preparation:
- Wash Hands: Before handling any sterile equipment, wash your hands thoroughly with soap and water.
- Prepare Your Supplies: Lay out the required materials on a clean surface. Ensure the dressing and other supplies are sterile.
- Put on Sterile Gloves: Wear gloves to reduce the risk of infection and contamination during the procedure.
2. Assess the Wound:
- Check the Wound Condition: Ensure the wound is clean and assess its size, depth, and exudate level. This will guide your choice of dressing type.
- Clean the Wound (if needed): Use sterile saline or wound cleanser to gently clean the wound if necessary. Make sure to remove any debris or old dressing.
3. Choose the Right Dressing:
Select a dressing based on the type and severity of the wound.
Common types include:
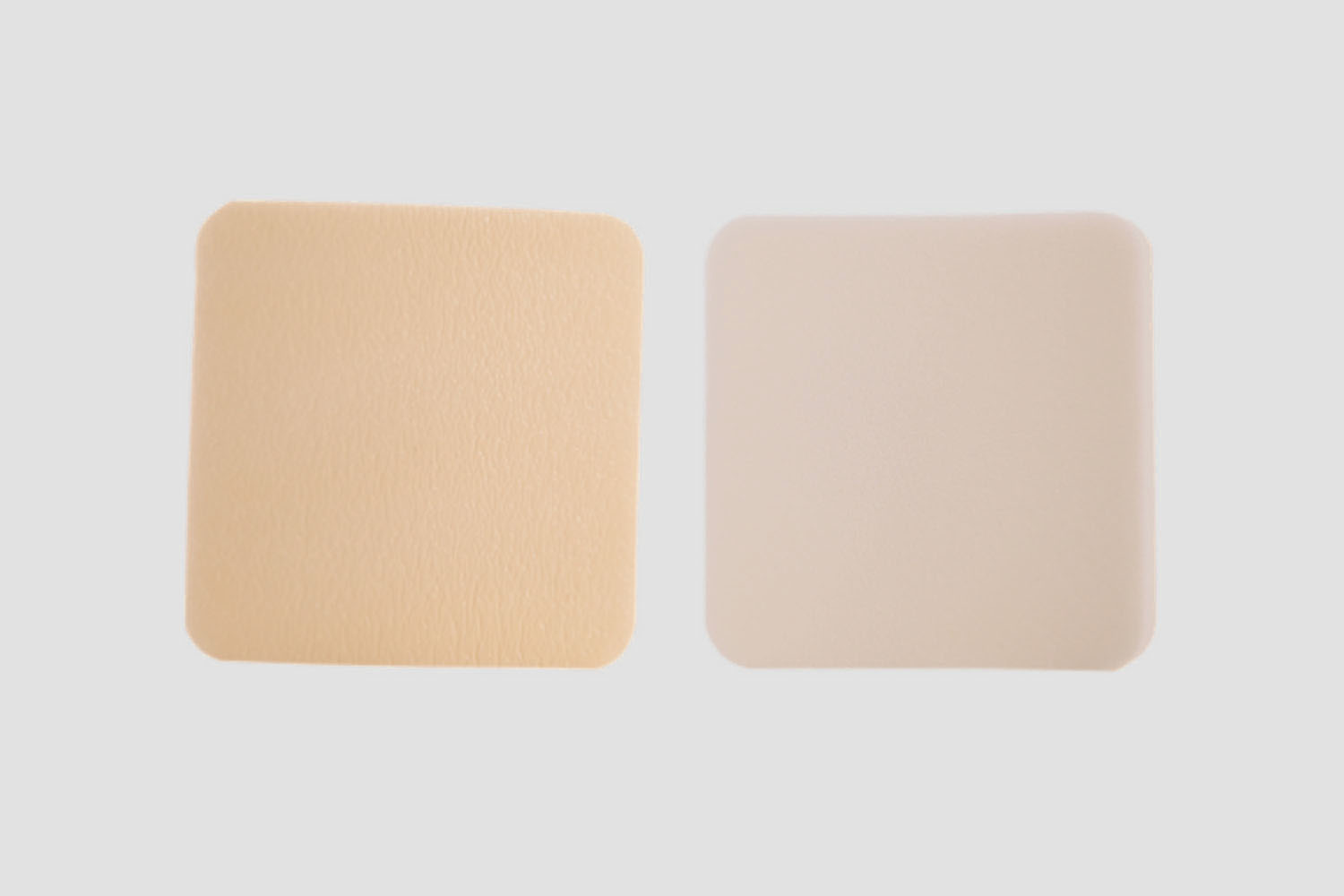
Hydrocolloid dressings for shallow, low-exudate wounds.
Foam dressings for moderate to high-exudate wounds.
Gauze pads for cleaning and absorbing light exudate.
Alginate dressings for heavily exudating wounds.
4. Apply the Dressing:
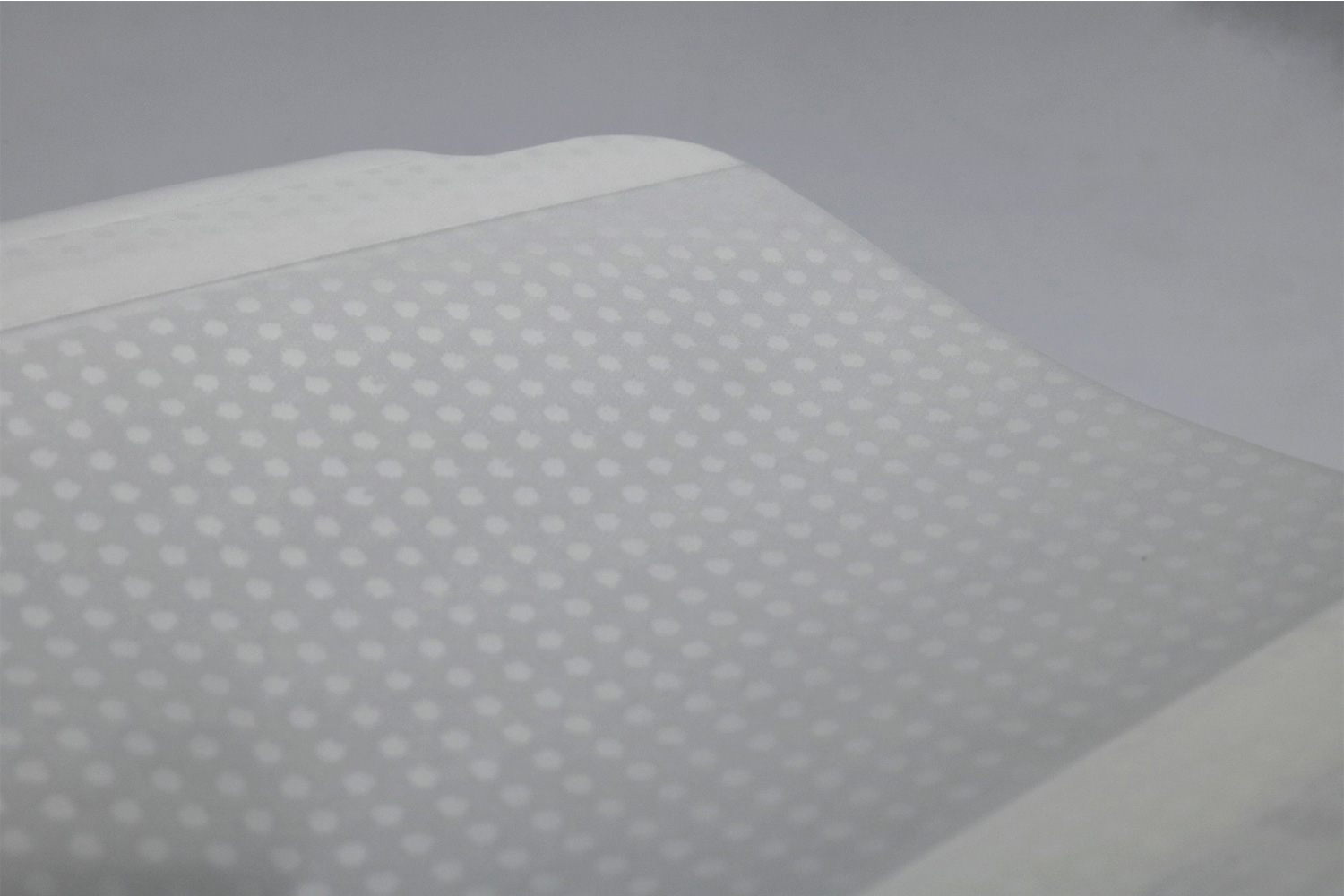
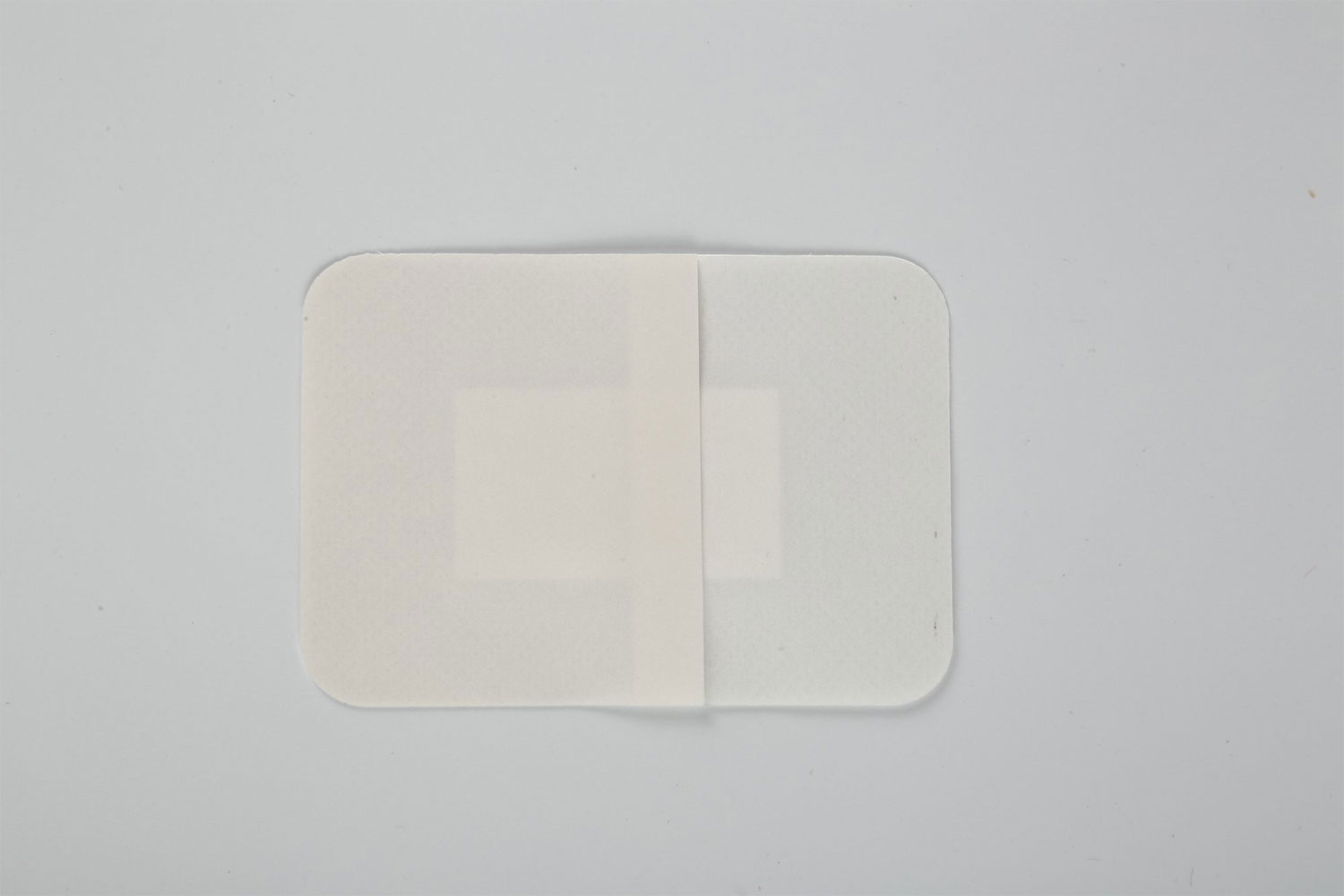
- Cut or Size the Dressing (if needed): If necessary, cut the dressing to match the size of the wound. It should cover the entire wound with a margin of healthy skin around the edges.
- Place the Dressing: Carefully place the dressing directly onto the wound without touching the sterile side. If using gauze, ensure it covers the wound thoroughly.
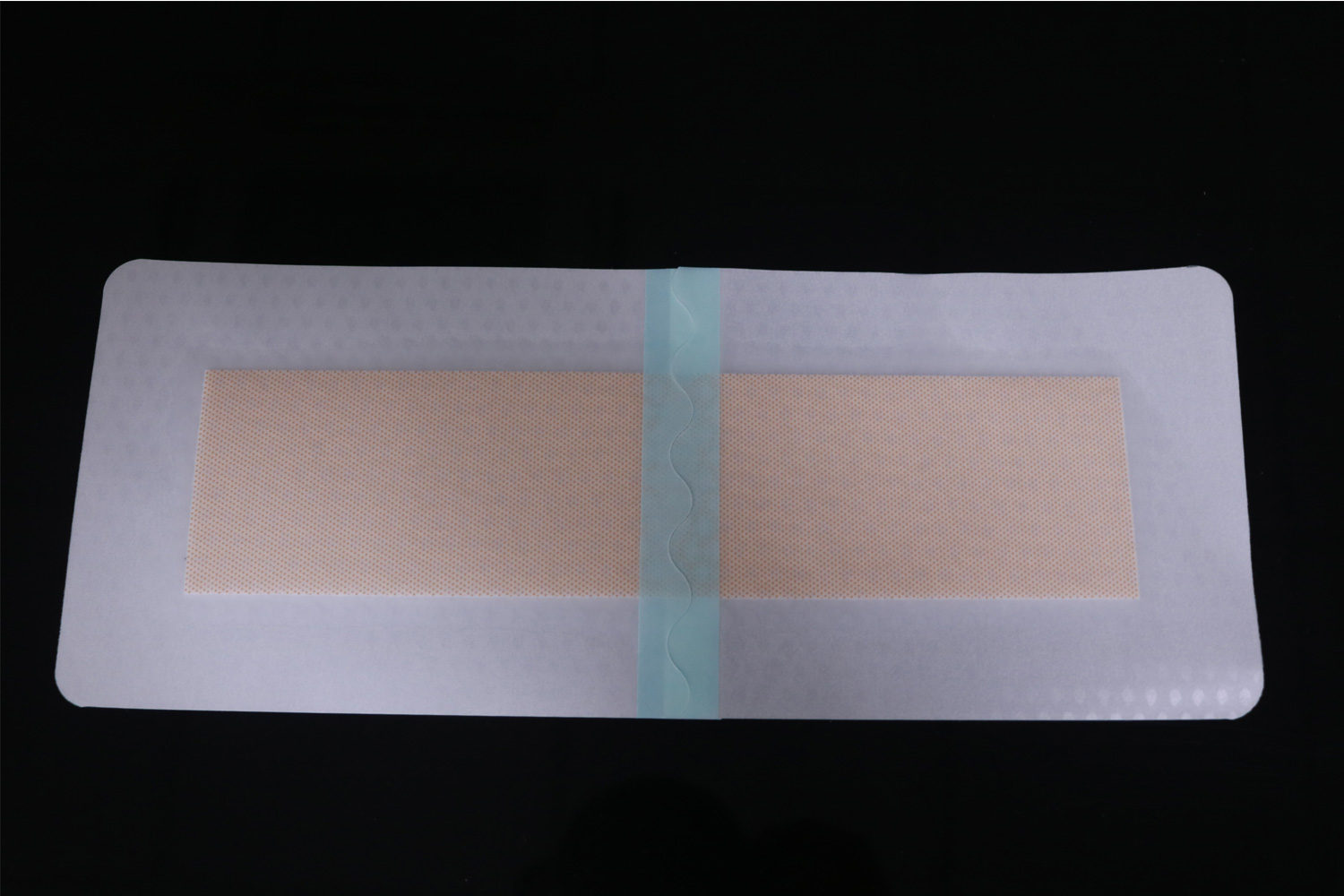
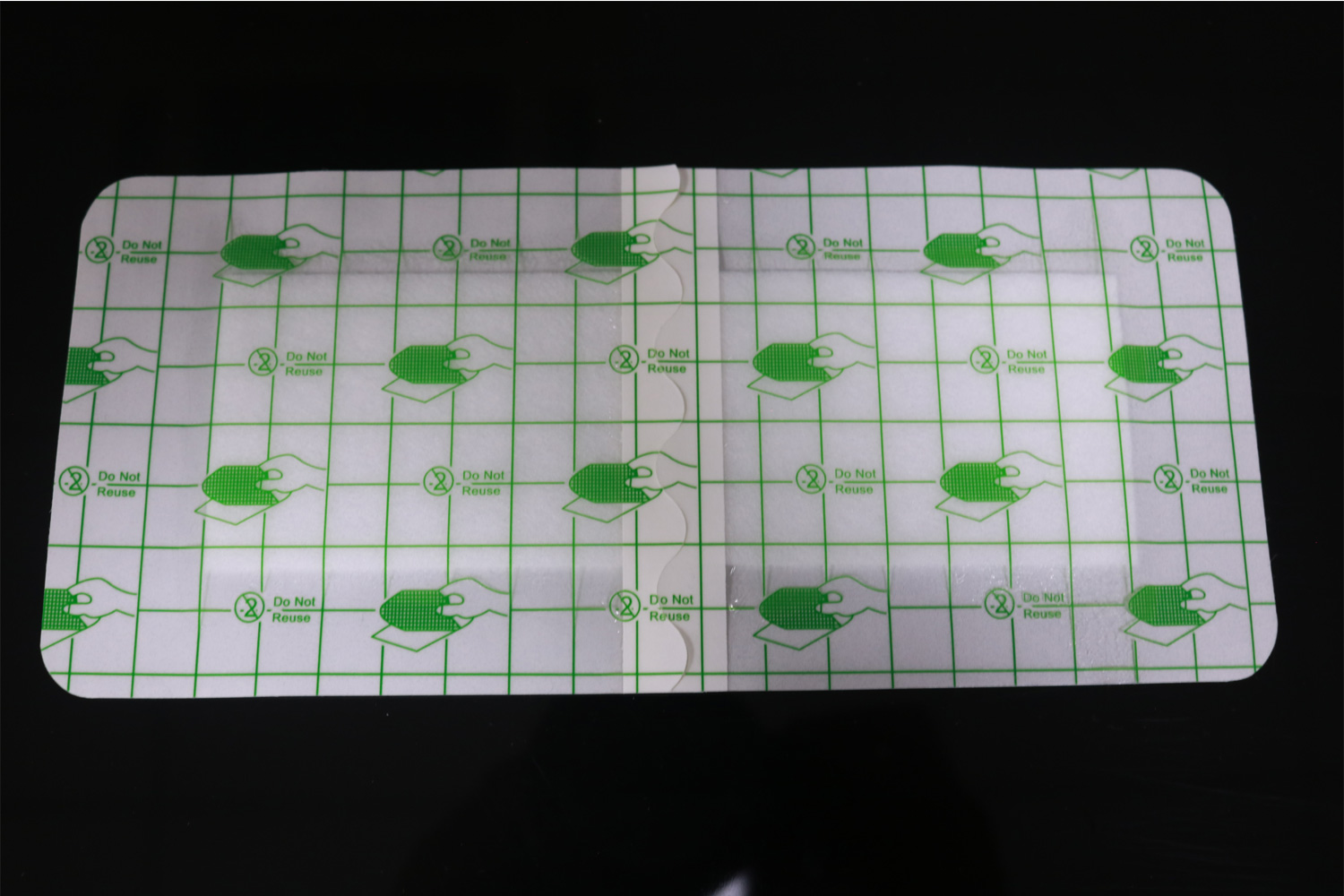
For hydrocolloid or foam dressings, remove any protective backing and gently apply it to the wound.
For gauze dressings, apply them directly over the wound and ensure the dressing stays in place without causing pressure on the wound.
5. Secure the Dressing:
Use adhesive tape, bandages, or mesh dressings to secure the dressing in place, depending on the type used.
Be careful not to tape too tightly to avoid restricting blood flow to the area.
If the dressing is self-adhesive, make sure it sticks well to the surrounding skin.
6. Dispose of Materials:
Dispose of used dressings, gloves, and any other disposable materials in an appropriate waste container, preferably one that is designated for biohazardous waste if the wound is potentially infected.
Wash your hands thoroughly after the procedure.
7. Monitoring and Follow-up:
- Monitor the Dressing Regularly: Depending on the type of dressing, it may need to be changed every 1-3 days, or more frequently if it becomes wet, soiled, or starts to lift from the skin.
- Assess for Infection: Watch for signs of infection, such as increased redness, swelling, heat, or discharge.
- Follow Medical Advice: Always follow the specific instructions from a healthcare provider regarding dressing changes and wound care.
General Tips:
Avoid touching the inside of sterile packaging or any part of the dressing that will touch the wound.
Use the appropriate dressing for the type of wound (e.g., do not use a highly absorbent dressing on a wound with minimal exudate).
Keep the wound dry when changing the dressing, unless otherwise instructed by a healthcare provider.
Following these steps can help ensure proper wound healing and minimize the risk of infection.